Abstract
Introduction
Allogeneic hematopoietic stem cell transplantation (HSCT) is a curative therapy for sickle cell disease (SCD) allowing a SCD-free survival over 95% among children with matched HLA-identical donor (Gluckman E. Blood, 2017; Bernaudin F. Haematologica, 2020). In adults, myeloablative HSCT is associated with more graft-versus host disease (GVHD) and higher toxicity (Cappelli B. Haematologica, 2019). More recent approaches using non myeloablative (NMA) conditioning regimen (3 gray (Gy) total body irradiation (TBI) plus alemtuzumab) followed by HLA-identical peripheral blood stem cells (PBSC) and post-transplant sirolimus appear safe in adults (Hsieh MM. JAMA, 2014), but incidence of graft failure might be higher than the one reported after myeloablative conditioning (MAC) (Alzahrani M. Br J Haematol, 2021). Here, we compare outcomes after MAC or NMA conditioning regimens in patients over 15 years old transplanted from a matched related donor (MRD).
Patients and methods
All consecutive patients transplanted for SCD from a MRD from January 2015 to October 2020 were eligible if they were over 15 years old and received a busulfan-based MAC conditioning regimen or a NMA conditioning regimen.
Chimerism was studied by analyzing various polymorphisms after polymerase chain reaction (PCR) amplification of DNA obtained from whole blood cells. Rejection was defined as donor chimerism <5%. Event-free survival (EFS) was defined as the probability to be alive with blood donor chimerism over 20%.
Results
Thirty-four patients were included: 20 in the MAC and 14 in the NMA groups. Median age at transplant was 17 years (range 15-46) without difference between groups. Forty four percent of patients had a history of cerebral vasculopathy, 79% of recurrent vaso-occlusive crises and 76% of acute chest syndrome. ABO major incompatibility was present in 15% of patients. There was no difference in patient characteristics according to the conditioning regimen group except for pre-transplant cerebral vasculopathy, more frequently reported in the MAC group: 70% versus 6% in the NMA group (p<0.001).
In the MAC group, conditioning regimen associated busulfan (12.8 mg/kg IV), cyclophosphamide (N=17) or fludarabine (N= 3) and anti-thymoglobulin (ATG, mostly 20mg/kg). Stem cell source was bone marrow and post-transplant immunosuppression combined cyclosporine and mycophenolate or methotrexate. In the NMA group, conditioning regimen associated 3Gy TBI and alemtuzumab (1mg/kg), followed by PBSC and post-transplant sirolimus.
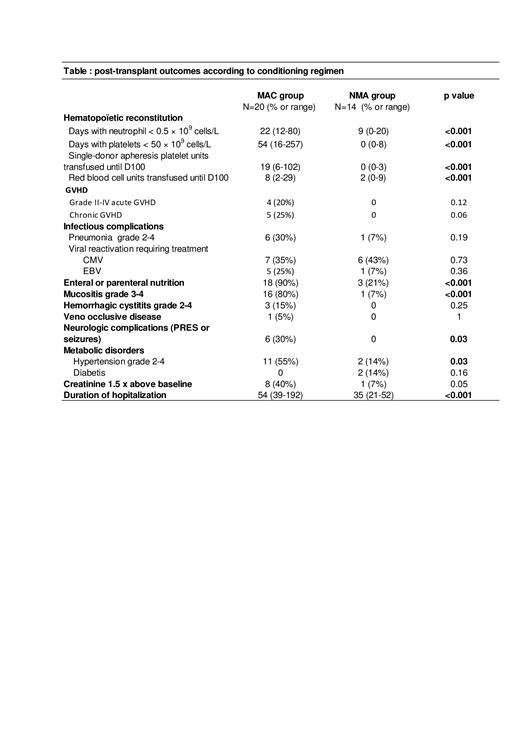
All patients engrafted and no secondary graft failure was observed. One MAC group patient died from GVHD. The 2-year overall and EFS were 95% (CI 95%: 85.9-100) in the MAC group (median follow-up of 39 months (range 8-63)) and 100% (CI 95%: 100-100) in the NMA group (median follow-up of 17 months (range 9-39)). Incidence of grade II-IV acute GVHD was 0% in the NMA group versus 20% in the MAC group (p=0.12). Incidence of chronic GVHD was 0% in the NMA group versus 25% in the MAC group (p=0.06). From the 27 patients with follow-up>12 months, 17/17 discontinued immunosuppressive therapy in the MAC group versus 8/10 in the NMA group. Hematopoietic recovery was faster in the NMA group with less platelet and red blood cell units transfused (Table). Throughout the follow-up, median donor chimerism was higher after MAC transplantation than after NMA transplantation: 98% (range 69-100) and 86 % (range 50-97) respectively at 1 year (p=0.017). Donor chimerism remained above 50% throughout the follow-up in all patients except 1 of the NMA group who displayed stable chimerism between 40 and 50%. All patients achieved HbS level close to the one of their donors. There was no difference between the 2 groups regarding occurrence of infections. MAC transplant was more often associated with hypertension, neurological complications, severe mucositis and need of enteral or parenteral nutrition. Moreover, duration of hospitalization was longer in MAC group: 54 days (range 39-192) versus 35 days in the NMA group (range 21-52) (p<0.001) (table).
Conclusion
In this series of adolescents and adults transplanted for SCD, the survival without SCD was excellent with a faster hematological recovery and a lower toxicity after NMA HSCT. Longer follow-up is required to confirm stable mixed donor chimerism and the cure of SCD after NMA approach.
Joseph: bluebird bio: Consultancy. Boissel: Servier: Consultancy, Honoraria; JAZZ Pharma: Honoraria, Research Funding; Incyte: Honoraria; Amgen: Consultancy, Honoraria, Research Funding; SANOFI: Honoraria; CELGENE: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria, Research Funding; PFIZER: Consultancy, Honoraria. Pondarré: ADDMEDICA: Honoraria.